platelet-rich plasma therapy
Platelet-Rich Plasma Therapy Offers Natural Relief and Rejuvenation
An effective, all-natural treatment with results that last.
In a market becoming saturated with medications and pharmaceutical treatments, it can be difficult to find solutions that offer what patients really want: effective results with few side effects.
Platelet-Rich Plasma (PRP) Therapy delivers.
By using growth factors from the platelets of a patient’s own blood, a healing response is triggered in the body. In an increasing number of studies, PRP Therapy is being shown to be a powerful, effective, and lasting solution for a wide variety of issues – from tennis elbow and frozen shoulder to plantar fasciitis and wound healing.
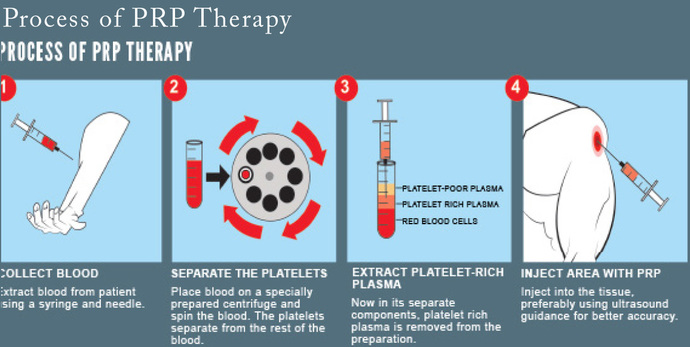
The process is simple with kits and a centrifuge from our vendor – just draw a blood sample, spin it down in the low speed centrifuge, extract the platelet-rich plasma, and inject it into the area of concern. The treatment is autologous and there are few, if any, contraindications.
PRP Therapy has been shown to be effective in both the orthopedic and aesthetic fields. When used as a treatment for tennis elbow, frozen shoulder or other joint related issues, results are both rapid and durable. Within a matter of weeks, patients report the reduction and often cessation of pain and discomfort and, unlike steroid treatments, this relief truly lasts.
In the treatment of aesthetic and aging issues, such as acne scarring, wrinkles, or hair restoration, PRP Therapy has been showing amazing results. And because this treatment is non-invasive, heals rapidly, and has no negative side effects, this is one solution that really works for your patients.
BACMAC is proud to offer an easy to implement, turnkey PRP Therapy solution. This procedure is becoming increasingly popular and, thanks to the simple process pioneered by the Yes PRP Kit, there has never been a better time to get started.
Who Can Benefit from PRP Therapy?
PRP initially gained popularity from its promise as a safe alternative to surgery with few contraindications. PRP has been proven in countless clinical studies to be effective in medical procedures where healing and cell regeneration are the treatment goal. Today, PRP is common in numerous specialties including, but not limited to:
Benefits of PRP Therapy
PRP offers many unique benefits for a wide range of practices, patients, and conditions. Here are just a few:
Key Cellular Components of Platelet-Rich Plasma
In order for PRP to be successful, platelets must be activated to successfully release their contents and begin the healing cascade and ultimate restoration of collagen.
Collagen repair can be separated into three phases:
An effective, all-natural treatment with results that last.
In a market becoming saturated with medications and pharmaceutical treatments, it can be difficult to find solutions that offer what patients really want: effective results with few side effects.
Platelet-Rich Plasma (PRP) Therapy delivers.
By using growth factors from the platelets of a patient’s own blood, a healing response is triggered in the body. In an increasing number of studies, PRP Therapy is being shown to be a powerful, effective, and lasting solution for a wide variety of issues – from tennis elbow and frozen shoulder to plantar fasciitis and wound healing.
The process is simple with kits and a centrifuge from our vendor – just draw a blood sample, spin it down in the low speed centrifuge, extract the platelet-rich plasma, and inject it into the area of concern. The treatment is autologous and there are few, if any, contraindications.
PRP Therapy has been shown to be effective in both the orthopedic and aesthetic fields. When used as a treatment for tennis elbow, frozen shoulder or other joint related issues, results are both rapid and durable. Within a matter of weeks, patients report the reduction and often cessation of pain and discomfort and, unlike steroid treatments, this relief truly lasts.
In the treatment of aesthetic and aging issues, such as acne scarring, wrinkles, or hair restoration, PRP Therapy has been showing amazing results. And because this treatment is non-invasive, heals rapidly, and has no negative side effects, this is one solution that really works for your patients.
BACMAC is proud to offer an easy to implement, turnkey PRP Therapy solution. This procedure is becoming increasingly popular and, thanks to the simple process pioneered by the Yes PRP Kit, there has never been a better time to get started.
Who Can Benefit from PRP Therapy?
PRP initially gained popularity from its promise as a safe alternative to surgery with few contraindications. PRP has been proven in countless clinical studies to be effective in medical procedures where healing and cell regeneration are the treatment goal. Today, PRP is common in numerous specialties including, but not limited to:
- Sports Medicine/Orthopedic
- Dentistry
- Otolaryngology
- Podiatry
- Neurosurgery
- Ophthalmology
- Urology
- Wound healing
- Cosmetic
- Cardiothoracic
- Maxillofacial surgery
Benefits of PRP Therapy
PRP offers many unique benefits for a wide range of practices, patients, and conditions. Here are just a few:
- Minimal risk
- Short recovery time
- Limited contraindications
- Cost-effective treatment
- Targeted and accelerated healing
- Rapid results with long-term benefits
- Natural, visible improvement without artificial enhancement
- High level of patient satisfaction
- Significant return on investment
Key Cellular Components of Platelet-Rich Plasma
- Platelets
- Monocytes
- Fibroblasts
- Osteoblasts
- Macrophages
- Keratinocytes
- Endothelial Cells
- Polymorphonuclear Neutrophils
In order for PRP to be successful, platelets must be activated to successfully release their contents and begin the healing cascade and ultimate restoration of collagen.
Collagen repair can be separated into three phases:
- Inflammation – Can last up to three days, as growth factors are released.
- Proliferation – Can last up to three weeks, as an influx of fibroblasts go to the injury site where differentiation and neovascularization occur.
- Remodeling – Can last up to one year, as new collagen matures and strengthens.
How Do I Get Started?
Platelet-Rich Plasma Therapy is gaining in popularity and acceptance due to its incredible results, its lack of adverse side effects, and the ease of treatment. Our solution offers the same promise – easy to implement and easy to use.
Our vendor, Zizion, will supply the slow-arm centrifuge and the kits necessary for treatment. You can then see the benefits of PRP Therapy first-hand.
A Revolutionary New Standard
Our Yes PRP Kit sets a new standard for quality and efficacy. When it comes to PRP Therapy, nobody does it better!
Here are a few reasons our kits stand out from the pack:
High-Quality, Slow Arm Centrifuge
If you find that PRP Therapy is not right for your practice at any time, simply return the centrifuge to Zizion and you will be refunded the full cost. However, if you choose to continue using Yes PRP Kits and order more kits to use in your practice, we will happily credit your practice the full amount of the centrifuge!
From Scientific American – “The Current Landscape”
Torn tendons, muscles and ligaments plague athletes in many types of sports. In attempts to help heal the wounded tissue, some athletes, both amateur and professional, have turned to platelet-rich plasma (PRP) therapy. For the treatment, doctors take a small vial of a patient’s blood, about 30 milliliters, and spin it in a centrifuge to separate the platelet-rich plasma from the other components. Then they inject the concentrated platelets at the site of the patient’s injury. In theory, the growth factors that platelets secrete (not including human growth hormone) spur tissue recovery.
Before playing in all four professional golf majors in 2015, Tiger Woods received four injections of PRP in his left knee following surgery. PRP injections in his elbow may have been the reason that Los Angeles Dodgers’s Pitcher Takashi Saito was able to return to the mound for the 2008 Major League Baseball playoffs.
Whereas doctors have used PRP therapy since the mid-1990s to aid bone healing after spinal injury and soft tissue recovery following plastic surgery, it has only been in the past year that the treatment has caught on for treatment of sports-related injuries. “PRP treatment really gained speed last January. It got press that two of the Pittsburgh Steelers [Hines Ward and Troy Polamalu] used it before [winning] the Super Bowl. More and more patients started to ask about it,” says Dennis A. Cardone, a doctor of osteopathic medicine at the New York University (N.Y.U.) Hospital for Joint Diseases. Cardone has treated 30 amateur athletes with PRP therapy over the past year.
ScientificAmerican.com spoke with N.Y.U.’s Cardone about what we know and don’t know about PRP therapy. [An edited transcript of the interview follows.]
What kinds of athletes have you treated over the last year with platelet-rich plasma (PRP) therapy?
They’ve been runners to basketball players to football players to collegiate competitive cheerleaders, a lacrosse player and a soccer player.
How could concentrating the platelets that are at the site of injury help healing?
Theoretically, many of the athletes may have a type of tendonitis, [such as] Achilles tendonitis or, say, patellar tendonitis in the knee or tennis elbow. Many of these tendon injuries become chronic, and involve microscopic tearing of the tendon and formation of scar tissue. A reason why it’s difficult to heal these tendon injuries is related to poor blood supply to the region. The perfect example would be the Achilles. It’s a tendon with, in general, a poor blood supply, so when there are these microscopic tears or chronic scarring, the body has a difficult time healing it. The theory is that the body can’t on its own get enough of these healing or growth factors to the area, but now this concentrated platelet injected there just enhances the nutrients and growth factors to allow the body to heal it.
You use the word “theory”. What kind of evidence is there that PRP helps heal tendonitis?
We all would like to see more evidence for this therapy. While there is some evidence, we still do not have the type of randomized, blinded, placebo-controlled studies that we would like to see. Most of the early literature has been poorly designed studies so we need better evidence about this treatment going forward. Ultimately we’d all like to see a study where we had 100 people with an Achilles tendonitis, 50 of them were injected with placebo and 50 of them were injected with PRP to really see if there was a difference.
The studies that have been performed have been, “Okay, let’s take 30 people with tennis elbow and let’s inject these 30 people with PRP therapy, and let’s follow them for a month and let’s see how they do.” So you’re just looking at this one population, you’re not comparing it to a control population [that receives an injection with placebo]. The thing about doing PRP therapy is that there are potentially other healers going on. Number one is there’s always potential for some type of placebo effect any time you put a needle in anyway. Number two is when you put a needle into a tendon, like you do for PRP therapy, you are likely to cause some bleeding and this is known to help healing [by bringing in more platelets]. So even by sticking a needle in a tendon and aggravating the tendon, you actually are helping the healing response.
Everyone looks at this one study that came out more than a year ago on tennis elbow but the problem is, it was a cohort study. Some people come in, they already know they want it, or there are patients that have failed other treatments. Any time we talk to anyone about PRP treatment, one of the first things that needs to be said is that, right now, there’s not good evidence to support the treatment.
Are any clinical trials currently going on?
Absolutely. In the next six months to a year, we should really start seeing results from many clinical trials, and hopefully good ones, ranging in everything from rotator cuff problems [in the shoulder] to tennis elbow to Achilles and patellar tendonitis.
It seems like there’s been many studies done on tissue grown in the lab and in lab animals [mice and rats]. Could you give me an idea of what those studies have told you about how well PRP therapy works?
Many of the studies early on are animal studies and lab studies. Many of those have been very positive for PRP in terms of tendon-healing effects. That’s part of that lack of evidence. It’s great that the animal studies look good but you need human studies.
How have your patients done on PRP therapy?
I would say, anecdotally, the whole population overall has done fairly well. There are a number that haven’t noticed much response and then there’s a good number that have done well. I think that’s why continue [to use it].
A good example is a patient that I have with an Achilles problem and he tried everything, everything, everything—went to other docs and he was all ready for surgery [to remove the scar tissue] and we did PRP therapy on him. He ended up with two sessions of therapy and he’s had a great cure that seems to be related to PRP. And then I’ve had some people, runners with chronic hamstring injury, and they will tell me they haven’t noticed a difference.
I’d probably say that maybe 60 percent of my patients do better.
Aesthetic Uses of PRP Therapy
Q: What is the process?
Preparation is simple and quick, and completed on the health care provider’s premises in the appointment time. Prior to treatment a simple blood sample of 10 – 20 mls is extracted from the patient. This blood is immediately placed in the centrifuge for 5 – 8 minutes. When centrifugation is complete the plasma will be separated from the red blood cells. The rich platelets are extracted from the base of the plasma gel. The platelets are injected into the deep dermis or fat layer of the skin. Platelets gradually increase collagen which can increase skin thickness and overall health of the skin
Q: Do I need a skin test?
No, PRP therapy is non-allergenic and autologous.
Q: Are results immediate?
No. Immediate swelling and wound healing are obvious at first sight. However, collagen rejuvenation can take from 6 weeks depending on the condition of your skin and lifestyle. More than one treatment will be necessary if the skin is mature. More then one treatment will be necessary if the skin is mature.
Q: How long do the results last?
As we are regenerating collagen, lasting results will depend on the care and maintenance of your skin. However, 2-3
treatments will help results last up to 18 months.
Q: How long is the process from start to finish?
Approx 45 minutes per two test tubes. One treatment can take as little as 20 minutes with the effective, efficient kit.
Q: Does the treatment hurt?
Regenerative medicine is administered via an injection. Topical or local anesthetics can be administered if needed.
Q: What facial and body areas can be treated?
Q: What can I expect after treatment?
Redness, swelling, slight pain, bruising or all these signs can happen in the treatment area. These side effects usually subside in a few hours to a few days. Post-care instructions need to be followed.
The Bottom Line
Platelet Rich Plasma Therapy is a powerful treatment option for your patients. It has a lasting regenerative effect, and the results last longer than other treatments’. It’s entirely natural and simple to perform – patients love it! Let’s outline how this benefits your practice.
Start-Up Costs
There are three options when you first order your PRP kits:
1) Trial Starter Pack:
Profits and Growth
PRP Therapy is currently covered by insurance for only a limited number of orthopedic issues and is being administered on a cash basis.
Recent Studies
The Effect of PRP on Cell Migration/Proliferation Rates of the HaCaT Keratinocyte Cell Line
We analyzed the effect of PRP on migration and proliferation rates of the HaCaT keratinocyte cell line. PRP treatment resulted in a dose-dependent increase of the proliferation rates of HaCaT cells. In addition, PRP treatment resulted in markedly increased rates of migration of HaCaT cells, even with a low concentration of PRP (0.005-0.5%).
Expression of cell cycle regulatory proteins in the HaCaT keratinocyte cell line by PRP treatment. Cell cycle regulatory proteins are important in proliferation and migration of HaCaT keratinocyte cell lines. We have investigated the question of whether PRP treatment promotes the proliferative and migratory activities of HaCaT cells through upregulation of G1/Sor G2/M transition regulatory proteins. In order to determine the basal expression levels of cell cycle regulatory proteins in HaCaT cells, cells were cultured without fetal bovine serum (FBS) for 3 days. After serum starvation for 3 days, cells were cultured under 5% FBS or 2% (v/v) PRP with DMEM. Expression levels of G1/S transition regulatory proteins, namely, ppRb, CDK4 and cyclin A, were decreased in serum-starved HaCaT cells. Notably, 2% PRP induced increased expression of cyclin A and CDK4 in HaCaT cells, resulting in increased expression of ppRb. Markedly increased expression of cyclin D1, cyclin E and CDK4 was not observed.
Wound Healing Effect of PRP on Acute and Chronic Skin Ulcers
Based on the laboratory data that support the enhancing effect of PRP on wound healing, we performed a clinical application of PRP to acute and chronic wounds and evaluated its clinical wound healing effect. Eleven patients with chronic ulcers (cases 1-11) presented with stasis ulcer, diabetic ulcer, venous leg ulcer, livedoid vasculitis, claw foot and traumatic ulcer. The mean period of the disease was 8.54 months. However, in 15.18 days, 9 patients showed 90-100% epithelization. Case 2 presented with large-sized stasis ulcers and had been refractory to standard treatment for 2 months. However, almost a complete epithelization was shown in 24 days after 3 PRP treatments at 3-day intervals. In case 4, the patient had been suffering from a penetrating non-adhesion deep ulcer on an amputated foot for 18 months. The wound had not been healed by sutures. Thus, we applied PRP gel (6 times) on the ulcer and observed a complete epithelization 20 days after treatment. In case 11, a round-shaped ulcer on the middle interphalangeal joint of the left 3rd toe following corn treatment using cryotherapy also showed epithelization in 23 days after treatment 3 times with PRP gel solution.
In 5 patients with acute ulcers (cases 12-16), an 80-100% epithelization rate was achieved in 20 days. These wounds had occurred for an average of 2 months, including special indications such as dehiscence, open wound, pressure ulcer and burn wound.
Three months after the treatment, the majority of the patients (90%), including acute and chronic patients, evaluated the ulcer appearance as having good to excellent improvement and the remaining patients (10%) rated the improvement as moderate.
Sung-Ae Kim, Han-Won Ryu, Kyu-Suk Lee and Jae-We Cho
Department of Dermatology, Keimyung University School of Medicine, Daegu 700-712, Republic of Korea
Received August 2, 2012; Accepted November 29, 2012
Platelet-Rich Plasma Therapy is gaining in popularity and acceptance due to its incredible results, its lack of adverse side effects, and the ease of treatment. Our solution offers the same promise – easy to implement and easy to use.
Our vendor, Zizion, will supply the slow-arm centrifuge and the kits necessary for treatment. You can then see the benefits of PRP Therapy first-hand.
A Revolutionary New Standard
Our Yes PRP Kit sets a new standard for quality and efficacy. When it comes to PRP Therapy, nobody does it better!
Here are a few reasons our kits stand out from the pack:
- Our system allows the blood sample to be spun at lower speeds. This means a much better yield of live, non-activated, viable platelets is obtained from each draw.
- We use ACDA (Anticoagulation Dextrose) instead of Gel to separate the plasma and red blood cells (RBCs).
- Kits are extremely easy to use.
- Doctor/Technician has total control of RBCs in sample.
- Yes, the PRP Kit is extremely cost effective.
High-Quality, Slow Arm Centrifuge
If you find that PRP Therapy is not right for your practice at any time, simply return the centrifuge to Zizion and you will be refunded the full cost. However, if you choose to continue using Yes PRP Kits and order more kits to use in your practice, we will happily credit your practice the full amount of the centrifuge!
From Scientific American – “The Current Landscape”
Torn tendons, muscles and ligaments plague athletes in many types of sports. In attempts to help heal the wounded tissue, some athletes, both amateur and professional, have turned to platelet-rich plasma (PRP) therapy. For the treatment, doctors take a small vial of a patient’s blood, about 30 milliliters, and spin it in a centrifuge to separate the platelet-rich plasma from the other components. Then they inject the concentrated platelets at the site of the patient’s injury. In theory, the growth factors that platelets secrete (not including human growth hormone) spur tissue recovery.
Before playing in all four professional golf majors in 2015, Tiger Woods received four injections of PRP in his left knee following surgery. PRP injections in his elbow may have been the reason that Los Angeles Dodgers’s Pitcher Takashi Saito was able to return to the mound for the 2008 Major League Baseball playoffs.
Whereas doctors have used PRP therapy since the mid-1990s to aid bone healing after spinal injury and soft tissue recovery following plastic surgery, it has only been in the past year that the treatment has caught on for treatment of sports-related injuries. “PRP treatment really gained speed last January. It got press that two of the Pittsburgh Steelers [Hines Ward and Troy Polamalu] used it before [winning] the Super Bowl. More and more patients started to ask about it,” says Dennis A. Cardone, a doctor of osteopathic medicine at the New York University (N.Y.U.) Hospital for Joint Diseases. Cardone has treated 30 amateur athletes with PRP therapy over the past year.
ScientificAmerican.com spoke with N.Y.U.’s Cardone about what we know and don’t know about PRP therapy. [An edited transcript of the interview follows.]
What kinds of athletes have you treated over the last year with platelet-rich plasma (PRP) therapy?
They’ve been runners to basketball players to football players to collegiate competitive cheerleaders, a lacrosse player and a soccer player.
How could concentrating the platelets that are at the site of injury help healing?
Theoretically, many of the athletes may have a type of tendonitis, [such as] Achilles tendonitis or, say, patellar tendonitis in the knee or tennis elbow. Many of these tendon injuries become chronic, and involve microscopic tearing of the tendon and formation of scar tissue. A reason why it’s difficult to heal these tendon injuries is related to poor blood supply to the region. The perfect example would be the Achilles. It’s a tendon with, in general, a poor blood supply, so when there are these microscopic tears or chronic scarring, the body has a difficult time healing it. The theory is that the body can’t on its own get enough of these healing or growth factors to the area, but now this concentrated platelet injected there just enhances the nutrients and growth factors to allow the body to heal it.
You use the word “theory”. What kind of evidence is there that PRP helps heal tendonitis?
We all would like to see more evidence for this therapy. While there is some evidence, we still do not have the type of randomized, blinded, placebo-controlled studies that we would like to see. Most of the early literature has been poorly designed studies so we need better evidence about this treatment going forward. Ultimately we’d all like to see a study where we had 100 people with an Achilles tendonitis, 50 of them were injected with placebo and 50 of them were injected with PRP to really see if there was a difference.
The studies that have been performed have been, “Okay, let’s take 30 people with tennis elbow and let’s inject these 30 people with PRP therapy, and let’s follow them for a month and let’s see how they do.” So you’re just looking at this one population, you’re not comparing it to a control population [that receives an injection with placebo]. The thing about doing PRP therapy is that there are potentially other healers going on. Number one is there’s always potential for some type of placebo effect any time you put a needle in anyway. Number two is when you put a needle into a tendon, like you do for PRP therapy, you are likely to cause some bleeding and this is known to help healing [by bringing in more platelets]. So even by sticking a needle in a tendon and aggravating the tendon, you actually are helping the healing response.
Everyone looks at this one study that came out more than a year ago on tennis elbow but the problem is, it was a cohort study. Some people come in, they already know they want it, or there are patients that have failed other treatments. Any time we talk to anyone about PRP treatment, one of the first things that needs to be said is that, right now, there’s not good evidence to support the treatment.
Are any clinical trials currently going on?
Absolutely. In the next six months to a year, we should really start seeing results from many clinical trials, and hopefully good ones, ranging in everything from rotator cuff problems [in the shoulder] to tennis elbow to Achilles and patellar tendonitis.
It seems like there’s been many studies done on tissue grown in the lab and in lab animals [mice and rats]. Could you give me an idea of what those studies have told you about how well PRP therapy works?
Many of the studies early on are animal studies and lab studies. Many of those have been very positive for PRP in terms of tendon-healing effects. That’s part of that lack of evidence. It’s great that the animal studies look good but you need human studies.
How have your patients done on PRP therapy?
I would say, anecdotally, the whole population overall has done fairly well. There are a number that haven’t noticed much response and then there’s a good number that have done well. I think that’s why continue [to use it].
A good example is a patient that I have with an Achilles problem and he tried everything, everything, everything—went to other docs and he was all ready for surgery [to remove the scar tissue] and we did PRP therapy on him. He ended up with two sessions of therapy and he’s had a great cure that seems to be related to PRP. And then I’ve had some people, runners with chronic hamstring injury, and they will tell me they haven’t noticed a difference.
I’d probably say that maybe 60 percent of my patients do better.
Aesthetic Uses of PRP Therapy
Q: What is the process?
Preparation is simple and quick, and completed on the health care provider’s premises in the appointment time. Prior to treatment a simple blood sample of 10 – 20 mls is extracted from the patient. This blood is immediately placed in the centrifuge for 5 – 8 minutes. When centrifugation is complete the plasma will be separated from the red blood cells. The rich platelets are extracted from the base of the plasma gel. The platelets are injected into the deep dermis or fat layer of the skin. Platelets gradually increase collagen which can increase skin thickness and overall health of the skin
Q: Do I need a skin test?
No, PRP therapy is non-allergenic and autologous.
Q: Are results immediate?
No. Immediate swelling and wound healing are obvious at first sight. However, collagen rejuvenation can take from 6 weeks depending on the condition of your skin and lifestyle. More than one treatment will be necessary if the skin is mature. More then one treatment will be necessary if the skin is mature.
Q: How long do the results last?
As we are regenerating collagen, lasting results will depend on the care and maintenance of your skin. However, 2-3
treatments will help results last up to 18 months.
Q: How long is the process from start to finish?
Approx 45 minutes per two test tubes. One treatment can take as little as 20 minutes with the effective, efficient kit.
Q: Does the treatment hurt?
Regenerative medicine is administered via an injection. Topical or local anesthetics can be administered if needed.
Q: What facial and body areas can be treated?
- Orbital Rim (around the eyes)
- Cheeks
- Saggy skin on the neck
- Back of hands
- Décolletage/Upper Female Torso
- Other Body Areas
Q: What can I expect after treatment?
Redness, swelling, slight pain, bruising or all these signs can happen in the treatment area. These side effects usually subside in a few hours to a few days. Post-care instructions need to be followed.
The Bottom Line
Platelet Rich Plasma Therapy is a powerful treatment option for your patients. It has a lasting regenerative effect, and the results last longer than other treatments’. It’s entirely natural and simple to perform – patients love it! Let’s outline how this benefits your practice.
Start-Up Costs
There are three options when you first order your PRP kits:
1) Trial Starter Pack:
- The trial program allows you to try the YES PRP system risk-free. You will have 30 days to use the system and upgrade to one of the packages listed below or return the centrifuge and unused product to receive a full refund.
- This package includes the FDA approved, swing arm, slow stop, centrifuge, and 30 YES PRP kits, along with content for your website, print-ready, digital files of promotional collateral with your logo and contact information, and print-ready posters. Networld On-Line will issue a joint press release announcing the addition of PRP to your practice, or your certification as a PRP Life Lift™ if you attend training and provide a detailed SEO report on your website.
- This package includes the FDA approved, swing arm, slow-stop centrifuge, and 50 PRP kits along with content for your website, print-ready, digital files of promotional collateral with your logo and contact information, and print-ready posters. Networld On-Line will issue a joint press release announcing the addition of PRP to your practice, or your certification as a PRP Life Lift™ if you attend training and provide a detailed SEO report on your website.
Profits and Growth
PRP Therapy is currently covered by insurance for only a limited number of orthopedic issues and is being administered on a cash basis.
Recent Studies
The Effect of PRP on Cell Migration/Proliferation Rates of the HaCaT Keratinocyte Cell Line
We analyzed the effect of PRP on migration and proliferation rates of the HaCaT keratinocyte cell line. PRP treatment resulted in a dose-dependent increase of the proliferation rates of HaCaT cells. In addition, PRP treatment resulted in markedly increased rates of migration of HaCaT cells, even with a low concentration of PRP (0.005-0.5%).
Expression of cell cycle regulatory proteins in the HaCaT keratinocyte cell line by PRP treatment. Cell cycle regulatory proteins are important in proliferation and migration of HaCaT keratinocyte cell lines. We have investigated the question of whether PRP treatment promotes the proliferative and migratory activities of HaCaT cells through upregulation of G1/Sor G2/M transition regulatory proteins. In order to determine the basal expression levels of cell cycle regulatory proteins in HaCaT cells, cells were cultured without fetal bovine serum (FBS) for 3 days. After serum starvation for 3 days, cells were cultured under 5% FBS or 2% (v/v) PRP with DMEM. Expression levels of G1/S transition regulatory proteins, namely, ppRb, CDK4 and cyclin A, were decreased in serum-starved HaCaT cells. Notably, 2% PRP induced increased expression of cyclin A and CDK4 in HaCaT cells, resulting in increased expression of ppRb. Markedly increased expression of cyclin D1, cyclin E and CDK4 was not observed.
Wound Healing Effect of PRP on Acute and Chronic Skin Ulcers
Based on the laboratory data that support the enhancing effect of PRP on wound healing, we performed a clinical application of PRP to acute and chronic wounds and evaluated its clinical wound healing effect. Eleven patients with chronic ulcers (cases 1-11) presented with stasis ulcer, diabetic ulcer, venous leg ulcer, livedoid vasculitis, claw foot and traumatic ulcer. The mean period of the disease was 8.54 months. However, in 15.18 days, 9 patients showed 90-100% epithelization. Case 2 presented with large-sized stasis ulcers and had been refractory to standard treatment for 2 months. However, almost a complete epithelization was shown in 24 days after 3 PRP treatments at 3-day intervals. In case 4, the patient had been suffering from a penetrating non-adhesion deep ulcer on an amputated foot for 18 months. The wound had not been healed by sutures. Thus, we applied PRP gel (6 times) on the ulcer and observed a complete epithelization 20 days after treatment. In case 11, a round-shaped ulcer on the middle interphalangeal joint of the left 3rd toe following corn treatment using cryotherapy also showed epithelization in 23 days after treatment 3 times with PRP gel solution.
In 5 patients with acute ulcers (cases 12-16), an 80-100% epithelization rate was achieved in 20 days. These wounds had occurred for an average of 2 months, including special indications such as dehiscence, open wound, pressure ulcer and burn wound.
Three months after the treatment, the majority of the patients (90%), including acute and chronic patients, evaluated the ulcer appearance as having good to excellent improvement and the remaining patients (10%) rated the improvement as moderate.
Sung-Ae Kim, Han-Won Ryu, Kyu-Suk Lee and Jae-We Cho
Department of Dermatology, Keimyung University School of Medicine, Daegu 700-712, Republic of Korea
Received August 2, 2012; Accepted November 29, 2012
To learn more, please call 800.240.9473 today.