The emphasis on try is an upfront admission that a blog post is not going to be the end-all and be-all answer. You aren’t going to read a 5000 word treatise on this – and I sure don’t want to write it.
With that caveat, here goes.
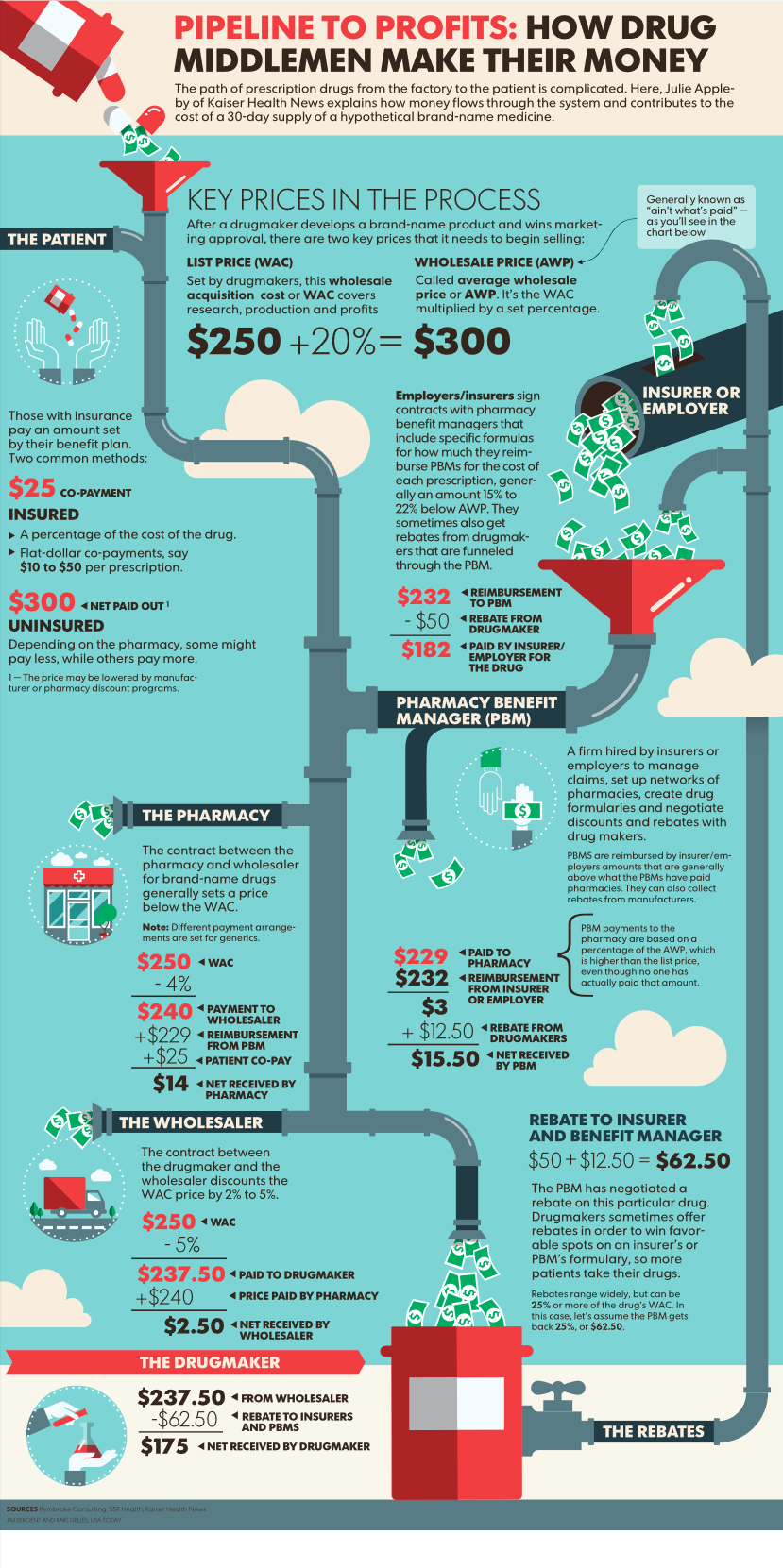
First up, we are dealing with intermediaries or middlemen. Think PBMs, bill review firms, networks; entities that contract with healthcare providers, pharmacies, durable medical equipment vendors, chiropractors etc.; also hospitals. The intermediaries aggregate buyers and providers and provide simple access to and communications, data, and financial flows between those entities.
Let’s take Pharmacy Benefit Management as an example. Of late large benefit buyers have been pushing PBMs to offer transparent pricing options. One, the National Drug Purchasing Coalition, is working with Express Scripts Inc. to provide its members with cost plus admin fee pricing for drugs. That is, buyers know and pay what ESI pays for drugs, plus a per-script admin fee. ESI won’t earn any fees from the dispensing pharmacies or it’s own mail order pharmacy, nor will it capture any rebate or similar revenue. (disclosure – ESI subsidiary myMatrixx is an HSA consulting client)
Express is also offering clients a choice of formularies; to quote the Washington Post, “…clients can choose between lists that include drugs with a high list price — and high rebate…or the new list with lower-price drugs but with little or no rebate.”
And that is one reason this whole transparency thing isn’t as easy or straight-forward as one may want.
Rebates – which in this example are payments from brand drug manufacturers to PBMs to financially incentivize the PBMs to offer their drugs – can be opaque and hard to pin down. Buyers demanding full transparency will want full financial credit for all rebates…but they may also want to keep total drug costs down.
In some cases, those buyers will find that those rebates they participate in mean their total drug costs are lower – while their members may pay more.
This is an admittedly simplistic scenario but one that illustrates the key question – what do buyers want when they say “transparency?” I’d suggest what many buyers want is lower cost – but they aren’t asking for lower cost, they are asking their vendors for a specific thing that the buyer thinks will reduce cost. Of course, they also want to know that they are getting a fair price.
After lots of analyses and back-and-forth data dumps and algorithm testing and forecasting, what usually happens is…the buyer picks a non-transparent pricing option, that usually has some cost-cap guarantee or other mechanism to manage risk.
What does this mean for you?
There’s a lot to unpack here – but my top three are:
- Ask for what you want as the end result, not a means to get there. Let the vendor figure out how to get you what you want.
- Transparency is defined different ways – make very sure your definitions are consistent within your organization and your vendor partners’.
- When you “go transparent” you’ll have to pay more for stuff your vendor was providing under a bundled price. Call centers, clinical support, formulary management, client and state reporting, script transfer programs…all cost money to deliver.

 RSS Feed
RSS Feed